Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a chronic, progressive respiratory disease that blocks airflow making it difficult to breathe. According to the World Health Organization, in 2016, COPD became the third leading cause of death in the world, and the fifth in high-income countries.
Medications and life-style changes help manage symptoms and slow the progression of COPD, however, new treatment approaches are needed to prevent or reverse ongoing damage to the lung.
What is COPD?
Chronic Obstructive Pulmonary Disease (COPD) is an umbrella term for a group of long-term lung diseases where the airways in the lungs become restricted making it difficult to breathe (see Figure 1).
Emphysema and chronic bronchitis are the most common conditions that make up COPD (see Figure 2). Many people with COPD have both of these conditions to some degree.
COPD is a progressive disease, meaning that lung function gets worse over time. Symptoms include shortness of breath, wheezing, coughing, chest tightness, or frequent respiratory infections. Symptoms may be mild at first, but as the disease progresses, these can become more constant, making it increasingly hard to breathe and consequently limit physical activity.
In response to triggers such as air pollution, allergens, or a chest infection, symptoms can worsen suddenly, described as a flareup or “exacerbation.”
The major cause of COPD is smoking, but it can also be caused by air pollution (including second-hand smoke), severe asthma, and repeated lung infections during childhood.
Figure 1: Respiratory System. When you breathe in, air flows in through the nose or mouth, down your windpipe (“trachea”) into passages called bronchial tubes or airways, and into the lungs. Inside the lungs, bronchial tubes branch out into thousands of tiny air sacs (“alveoli”) which expand like balloons as air enters. Oxygen moves through the very thin walls of the air sacs and into the blood in surrounding blood vessels. Carbon dioxide is returned out of the blood into the air sacs and exhaled as you breathe out. © logo3in1 / Adobe Stock.
Figure 2: Chronic Obstructive Pulmonary Disease (COPD) is a group of lung diseases that make it difficult to breathe. A. Emphysema causes alveolar air sacs to become damaged and stiff. Air gets trapped in the alveoli, making it hard to exhale. B. Chronic bronchitis causes swelling in the airways and an increase in mucus. This excess mucus makes it harder to breath and leads to a chronic cough. © tolgasez33 / Adobe Stock.
How is COPD treated?
Currently, treatments for COPD aim to relieve symptoms, prevent complications, and slow disease progression. There is no cure for COPD.
Treatments include medications that can reduce symptoms and cut down on flare-ups. These should be combined with self-care approaches such as a healthy diet, regular exercise, and stopping cigarette smoking. Each person’s COPD is different and treatment is tailored based on specific symptoms and how advanced the disease is. Treatments include:
Bronchodilators to relax the muscles around the airways which helps keep them open;
Anti-inflammatory drugs (steroids or corticosteroids) to decrease swelling and mucus production;
Antibiotics to fight bacterial infection;
Vaccination to help protect against the flu and pneumonia;
Supplemental oxygen, to raise oxygen levels in the blood if they are too low;
Lung surgery or lung transplantation may be considered if symptoms are severe. However, not everyone is a candidate and not everyone will benefit from this.
There are currently no treatments that prevent or correct the progressive tissue damage in lung disease
How are we using stem cells to understand COPD?
The lung has a complex three-dimensional structure, which is critical for its function. It is made up of many different specialized cell types that each perform their own job but work together to carry out the main lung function—to bring oxygen into the body and send carbon dioxide out. It is critical that oxygen is delivered to our cells so that they can produce the energy that is necessary for them to properly function.
In the bronchial tubes, there are cells that make and secrete mucus, and there are other cells with tiny hair-like structures (“cilia”) on the surface that sweep the mucus, along with trapped dust, viral particles, or bacteria, back up and out of the lungs. In the air sacs, there are cells involved in oxygen exchange, interspersed with cells that make lung surfactant that prevents the alveoli from collapsing when we breathe out. In addition to these cells that make up the lining of the airways and air sacs, the lung contains blood vessel, muscle, and immune cells.
Researchers are studying how our lungs first develop, how they are maintained and repaired throughout our life, and what goes wrong during the initiation and progression of lung diseases such as COPD.
Three-dimensional organ-like structures grown in the lab called organoids that mimic essential aspects of lung airway function are a particularly valuable tool for these studies, allowing researchers to study human lung development and adult lung function in greater depth. Lung organoids can be grown from several different cell sources:
Adult lung stem or progenitor cells from small pieces of lung tissue (e.g. from biopsies from patients)
Embryonic stem cells, cells derived from embryos that can give rise to all cells in the body
Induced pluripotent stem cells, adult tissue-specific cells that are reprogrammed in the lab to behave like embryonic stem cells. These cells have the capacity to become any cell type in the body.
Researchers are exploring how different specialized lung cells develop and how they talk to each other. Lung organoids are also being used to find new drugs to treat lung disease.
As organoids grown from biopsy and induced pluripotent stem cells are genetically identical to the patient or healthy donor, they can help researchers understand how genetic differences lead to variations in people’s susceptibility to disease or how they respond to different drugs.
Further, stem cell research is providing insight into how the lung normally responds to maintenance needs or injury. Researchers have identified cells in the lining of the bronchial tubes and air sacs that can serve as “localized stem cells,” that is, these cells can self-renew (make copies of themselves) and generate the specialized lung cell types found nearby. This work suggests that there are several different types of lung stem or progenitor cells in adults that are important for repairing different types of damage.
These findings have important implications for developing new stem cell and regenerative medicine approaches for lung diseases like COPD, that aim to halt or reverse the damage to the lungs.
What is the potential for stem cells to treat COPD?
Researchers are exploring the following stem cell and regenerative medicine approaches for the treatment of lung diseases such as COPD:
Harnessing native repair mechanisms. Researchers are looking for ways to take advantage of the lung’s existing repair mechanisms. They are studying the signals that switch on lung repair pathways in a normal lung with the ultimate goal to find new treatments that could activate this process in patients with lung diseases. Given the complexity of the lung and its repair mechanisms, and the complexity of diseases like COPD, there is still a lot to learn.
Cell-based therapies replacing lung cells lost and damaged in disease. In COPD, the cells that line the bronchial tubes and the thousands of tiny air sacs (“alveoli”) in the lungs are damaged and do not function properly. The idea of a cell-based therapy would be to generate replacement cells in culture and deliver these to the lungs.
Researchers are rapidly improving ways to generate these cells. It will also be important to deliver cells to the lung in a way that will allow them to integrate into the lining of the lung airways and air sacs to carry out their job.
Addressing chronic inflammation. Airway inflammation is a consistent feature of COPD and is linked to the disease getting worse. Researchers are working to better understand how inflammation is triggered, why it persists, and what can be done to break the cycle.
Some clinical trials have used Mesenchymal Stromal Cell-based therapies (MSCs; sometimes referred to as Mesenchymal Stem Cells) to try to reduce inflammation in lung diseases. As noted below, it is not clear yet whether this approach will be effective.
Building replacement lung tissue. There have been exciting advances in bioengineering lung tissue—that is, using various engineering and/or cell biology methods to grow three-dimensional lungs in the lab—with the eventual hope to make tissue robust enough for transplantation.
Engineers and scientists are using scaffolds to recreate the lung’s shape and adding lung cells that can grow on this. They continue to address the challenges in fully recreating the complex structure of the lung with its with its many different cell types and connections to other tissues, that all play a role in effective lung function.
What is the clinical status of cell-based therapies for COPD?
Currently, all cell therapy approaches for the treatment of COPD are experimental. While some approaches are promising, cell therapies have not yet been proven to benefit patients with COPD.
There have been a small number of early-phase clinical trials using cell-based therapy for a range of lung diseases, including COPD, that have been approved and regulated by a regulatory agency (such as the US Food and Drug Administration, FDA). These have mostly used Mesenchymal Stromal Cells (MSCs; sometimes referred to as Mesenchymal Stem Cells) from a range of tissue sources and have focused on testing safety in a small number of patients. In some cases, researchers reported a decrease in signs of inflammation. However, there is no clear evidence that MSC therapy improves lung function or quality of life.
These studies are very hard to compare. First, not all MSCs are the same. Their characteristics depend on where in the body they come from and how they are isolated and grown. Different studies have used cells from different sources. In addition, they have measured different outcomes, doses (number of cells), and ways to deliver the cells to the patient. A lot more work is needed to learn more about the biology of MSCs and to use this knowledge to develop standard methods and measurements for testing as a treatment for COPD.
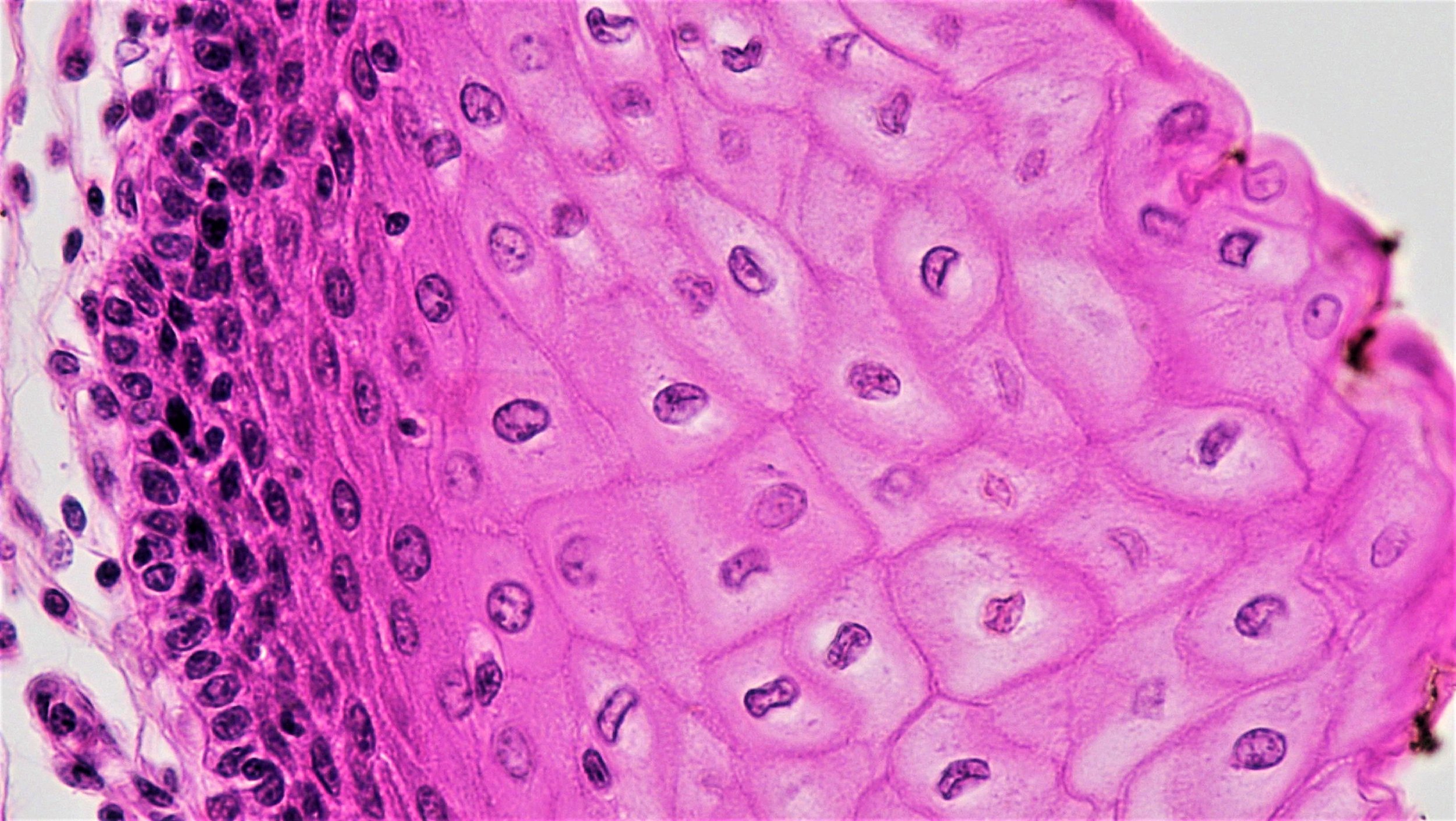
Epithelial cells
As described above, researchers are exploring the delivery of replacement cells that line the lung airways and air sacs. Scientist believe this approach may be more likely to be effective but, so far, it has only been tested in animals. Before this approach is ready to be tested in humans in clinical trials, researchers need to know more about how to grow the right cells, as well as the best conditions for delivering the cells to the lungs, so that the cells integrate properly and help improve lung function.
Concerns
Unfortunately, there are clinics selling unproven cell therapies or offering them as part of a clinical “study” outside of appropriate regulatory oversight. These clinics often make claims that are not backed up by facts. Before considering a cell-based treatment for COPD, even a clinical study or trial, take the time to learn more.
Read more about what lung specialists and patient groups recommend.
On our site, learn about red flags, such as high costs, and things to consider when thinking about participating in a clinical trial.
Useful Links
October 2019