Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic lateral sclerosis (ALS) is a progressive nervous system disease where the nerve cells in the brain and spinal cord that control the muscles die, causing an increasing loss of muscle control and ultimately death due to loss of control of muscles required to breathe. There is no cure for ALS yet, however, our understanding of what happens in ALS is advancing and pointing toward possible new treatments. Stem cells are a powerful tool for research into the causes and potential treatments for ALS.
What is ALS?
Amyotrophic lateral sclerosis (ALS) is a disease that involves the death of motor neurons in the brain and spinal cord that control our voluntary movement, such as walking, talking, and breathing.
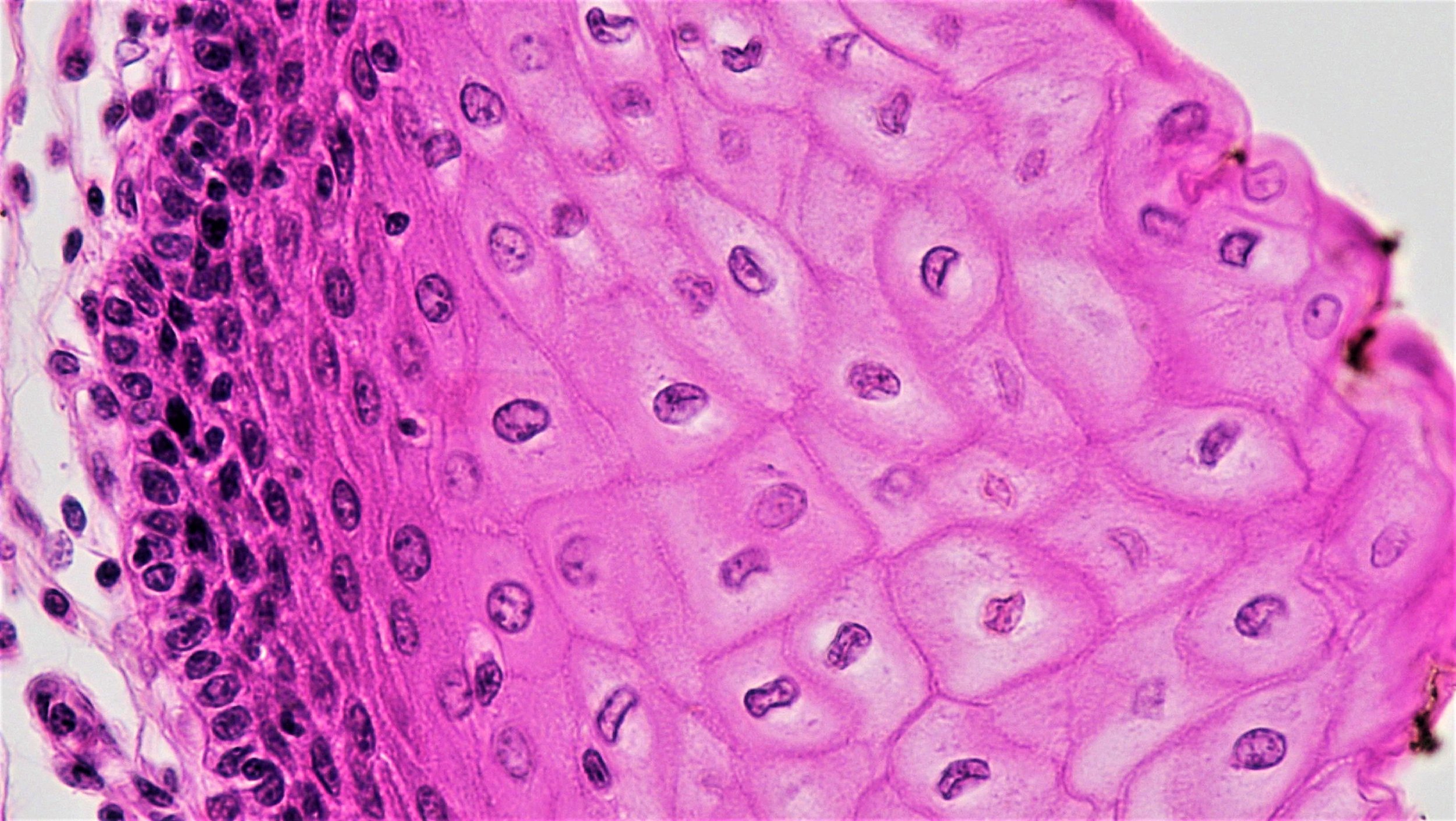
Our motor neurons are key in coordinating the movements of our muscles and certain organs throughout the body. These neurons reach from the brain to the spinal cord, and from the spinal cord to various muscles. These motor neurons carry the signals that control muscular movement. In ALS, motor neurons in both the brain and spinal cord begin to deteriorate and die and the muscles, without normal stimulation, gradually weaken and waste away. Eventually, the brain loses its ability to initiate movement or control the muscles.
The way in which ALS begins and progresses is variable from person to person. The first sign for some people is weakness in the hands, arms, or legs, for example experiencing difficulty grasping a pen or stumbling. Others may first notice a problem with speech or swallowing. The sequence of symptoms and the rate at which ALS progresses can be quite different; however, all people with ALS experience progressive muscle weakness and over time, become unable to move, talk, swallow, and eventually breathe.
The causes of ALS are not fully understood but a mix of genetic and environmental triggers are thought to be involved.
For about 10% of people with ALS, there is a family history or other evidence of a genetic change that contributes to the onset and progression of ALS. This is sometimes referred to as “familial” ALS. Mutations in several different genes have been found to play a role in the disease. For the majority of ALS cases, however, there is no apparent family history, and it is not clear what the triggers are.
The different ways in which people are affected and the different causes of the disease mean that ALS is not easy to diagnose. There is no single test to confirm ALS. A diagnosis of ALS is generally reached through physical examination and a series of tests, often ruling out other conditions that have similar symptoms.
Normally, the brain sends signals via nerve cells known as motor neurons to coordinate muscle movement throughout the body. In ALS, motor neurons deteriorate and then die. These neurons are no longer able to control muscle function and patients experience a range of debilitating motor symptoms.
How is ALS currently treated?
There is currently no cure for ALS. Current treatment approaches focus on managing symptoms and maintaining strength and quality of life.
Treatment for ALS is often multi-disciplinary, with care from a range of specialties such as neurology, physical therapy, and social work. Depending on symptoms and progression, a treatment plan may include:
A drug that slows progression of the disease: currently, these drugs do not reverse the damage already done to neurons but aim to provide protection against further damage and to slow the decline of physical function. Typically, the effects are limited, and may not be the right choice for everyone.
Other medications that address individual symptoms, such as muscle relaxants to ease cramps or drugs that decrease saliva production.
Physical therapy to reduce stiffness and discomfort and to maintain muscle strength
Support for speech, swallowing, and nutrition
Tools and devices to support communication and mobility
Breathing support
How are we using stem cells to understand ALS?
The cells affected by ALS are located in the brain and spinal cord and are difficult to access and examine closely in people living with the disease. Scientists have used stem cells to develop ways to recreate, or “model” ALS in the lab.
In particular, induced pluripotent stem cells, are being used in many laboratories studying ALS. Cells from the skin or blood can be reprogrammed or “induced” to an embryonic-like state and can then be coaxed to become any cell type in the body, including motor neurons and other cell types found in the brain and spinal cord. Scientists have made induced pluripotent stem cells from many different patients with ALS as well as from healthy individuals. These induced pluripotent stem cells grow indefinitely in the lab and can be used to generate large numbers of motor neurons with the same genetic makeup as the individual they were made from.
Scientists are using stem cells to:
Understand ALS and its causes: Scientists are studying what is happening inside and around the motor neurons that causes them to deteriorate and die in ALS and how this damage might be prevented or halted. They are studying why particular gene mutations cause ALS and what is taking place in patients with sporadic ALS, where there is not a clear genetic cause. Scientists are also examining how different cells of the nervous system influence each other as well as how they connect with muscle cells.
Improve diagnostic tools: Researchers have derived induced pluripotent stem cells from many different ALS patients, some with known genetic causes, others where there is no clear cause. Scientists are searching for what is common and what is unique about different patients. This information may help find ways to diagnose ALS more quickly and to better predict how an individual’s disease may progress or respond to particular treatments.
Identify and test new drugs: Motor neurons can be generated from induced pluripotent stem cells in large numbers, which allows scientists to screen for new drugs to treat ALS. They can test whether a drug slows down the deterioration of the motor neuron cells and compare this effect between patients with different underlying causes of ALS.
Develop cell-based approaches for the treatment of ALS: With the great progress in being able to generate neurons in the lab, scientists and doctors have explored how to generate healthy neurons to replace those that deteriorate in ALS. But there are major hurdles to this approach. The motor neurons would need to be delivered to the right places in the brain and along the spinal cord, and once there, they would need to connect to the existing network of neurons as well as signal to the muscles.
Given these challenges, the cell-based approaches being tested at the moment aim to slow down the progression of ALS by providing nourishment and protection to the existing motor neurons or by reducing inflammation in the brain and spinal cord tissue. These types of cell therapies will be further explored below in the next section.
What is the clinical status of cell-based therapies for ALS?
There are a number of small clinical trials that are using cell-based approaches to try to slow the progression of ALS. While some of these approaches are promising, cell-based therapies are still experimental. Follow-up trials are needed to fully understand any potential benefit for patients.
Replacement motor neurons
At this time, there are no clinical trials that aim to replace the motor neurons that die in ALS. As described above, researchers can generate motor neurons in the lab, as well as other cell types impacted by ALS. However, there are significant challenges in delivering replacement motor neurons to the right place and in their making the right connections with the muscle and other neurons. Nonetheless, stem cell-derived motor neurons are proving very valuable in finding and testing new drugs for ALS.
Support for existing neurons
There are a number of trials that have used stem cells to try to slow disease progression in ALS. These have generally used mesenchymal stromal cells (MSCs; sometimes referred to as Mesenchymal Stem Cells) that are taken from the bone marrow, grown in the lab, and then transplanted into the cerebral spinal fluid (CSF). In some cases, researchers have reported that there may be some positive effect—however, most of these trials have focused on testing safety in a small number of patients, and any observed benefit still needs to be confirmed in later-phase trials.
How might the cells help slow progression of ALS? Some MSCs have been shown to make neurotrophic factors, that is, proteins that support the growth and survival of neurons. They may also help reduce inflammation. These cells only last for a few months, so this process needs to be repeated.
There is also a trial underway using neural progenitor cells (brain-specific stem cells) that have been genetically engineered to release a supportive factor called glial cell-derived neurotrophic factor, or GDNF, which supports the survival and growth of motor neurons. These cells are intended to release GDNF for the lifetime of the patient.
Reducing inflammation: “Tregs”
Inflammation accompanies the death of motor neurons in ALS and may add to the damage over time. Doctors are testing a cell-based approach that takes advantage of the body’s regulatory T cells, also called Tregs, which have a role in decreasing inflammation and supporting healing after tissue damage. The patient’s own Tregs are taken, increased in number outside of the body, and then returned back to the patient, to see whether they will slow the progression of ALS.
Considerations for cell-based therapies and clinical trials
While there are a number of clinical trials ongoing and some are moving into later-stage phases, more testing is needed to know whether these cell-based treatments for ALS will be beneficial.
There are many centers globally that are involved with research and trials for ALS, and there are many ways for you to be involved:
Be counted! Look into joining a registry, for example, the CDC ALS Registry or the MND Register of England, Wales, and Northern Ireland.
Be connected! Find an ALS/MND network near you to learn more about local support and opportunities for patients and families.
Be aware! Unfortunately, there are clinics selling unproven cell therapies or offering them as part of a clinical “study” outside of appropriate regulatory oversight. Before considering a cell-based treatment for ALS, even a clinical study or trial, take the time to learn more about red flags, such as high costs, and things to consider when thinking about participating in a clinical trial.
Useful Links
April 2019