9 Things to Know About Stem Cell Treatments
⚠ Many clinics offering stem cell treatments make claims that are not supported by a current understanding of science.
Stem cells have tremendous promise to help us understand and treat a range of diseases, injuries and other health-related conditions. Their potential is evident in the use of blood stem cells to treat diseases of the blood, a therapy that has saved the lives of thousands of children with leukemia; and can be seen in the use of stem cells for tissue grafts to treat diseases or injury to the bone, skin and surface of the eye. Important clinical trials involving stem cells are underway for many other conditions and researchers continue to explore new avenues using stem cells in medicine.
There is still a lot to learn about stem cells, however, and their current applications as treatments are sometimes exaggerated by the media and other parties who do not fully understand the science and current limitations, and also by “clinics” looking to capitalize on the hype by selling treatments to chronically ill or seriously injured patients. The information on this page is intended to help you understand both the potential and the limitations of stem cells at this point in time, and to help you spot some of the misinformation that is widely circulated by clinics offering unproven treatments.
It is important to discuss these Nine Things to Know and any research or information you gather with your primary care physician and other trusted members of your healthcare team in deciding what is right for you.
1. Currently, very few stem cell treatments have been proven safe and effective.
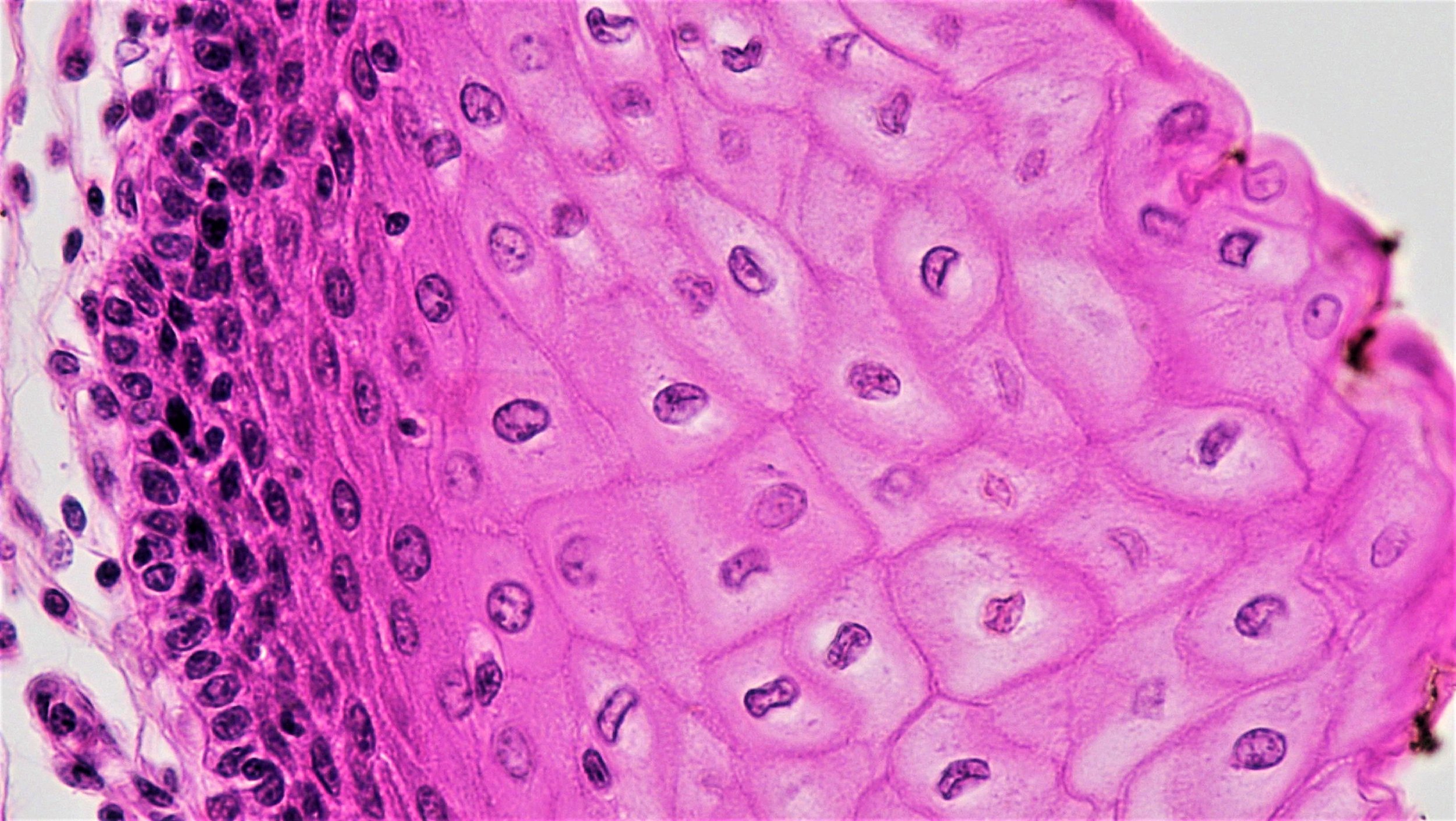
The list of diseases for which stem cell treatments have been shown to be beneficial is still very short. The best-defined and most extensively used stem cell treatment is hematopoietic (or blood) stem cell transplantation, for example, bone marrow transplantation, to treat certain blood and immune system disorders or to rebuild the blood system after treatments for some kinds of cancer.
Some bone, skin and corneal (eye) injuries and diseases can be treated by grafting or implanting tissues, and the healing process relies on stem cells within this implanted tissue. These procedures are widely accepted as safe and effective by the medical community. All other applications of stem cells are yet to be proven in clinical trials and should be considered highly experimental.
⚠ Caution: Beware of stem cell treatments offered without regulatory approval or outside the confines of a legitimate and registered clinical trial.
2. There is something to lose when you try an unproven stem cell “treatment”.
When there is no existing or effective treatment for a disease or condition, it is easy to understand why you may feel there is nothing to lose from trying something new, even if it isn’t proven. Unfortunately, most of the unproven stem cell “treatments” for sale throughout the world carry very little promise of actual benefit and very real risks:
Complications may create new short- and long-term health problems, and/or may make your condition or symptoms more difficult to manage.
Receipt of one unproven or experimental treatment may make you ineligible for future clinical trials or treatment options.
Out-of-pocket expenses could be enormous. In addition to treatment costs, there may be accommodation charges or other fees. In most cases, insurance companies and government health programs do not cover the cost of experimental treatments.
If travel is involved, there are additional considerations, including time away from friends and family.
Before you decide whether to pursue an unproven or experimental treatment, carefully assess the treatment you are considering. Weigh the risks and potential benefits. Get input from your loved ones and from your healthcare team; they may provide insight you haven’t thought of.
⚠ Caution: Unproven treatments present serious health, personal and financial considerations. Consider what might be lost and discuss these risks with your family and healthcare providers.
3. Different types of stem cells serve different purposes in the body.
Different types of stem cells come from different places in your body and have different functions. Learn more about various types of stem cells here.
Scientists are exploring the different roles tissue-specific stem cells might play in healing, with the understanding that these stem cells have specific and limited capabilities. Without manipulation in the lab, tissue-specific stem cells can only generate the other cell types found in the tissues where they live. For example, the blood-forming (hematopoietic) stem cells found in bone marrow regenerate the cells in blood, while neural stem cells in the brain make brain cells. A hematopoietic stem cell won’t spontaneously make a brain cell and vice versa. Thus, it is unlikely that a single cell type can be used to treat a multitude of unrelated diseases involving different tissues or organs.
⚠ Caution: Be wary of clinics offering treatments with stem cells originating from a part of your body unrelated to your disease or condition.
4. The same stem cell treatment is unlikely to work for different diseases or conditions.
Because stem cells that are specific to certain tissues cannot make cells found in other tissues without careful manipulation in the lab, it is very unlikely that the same stem cell treatment will work for diseases affecting different tissues and organs within the body.
Scientists have learned to make certain specialized cell types through a multi-step processes using pluripotent stem cells, that is embryonic stem cells or induced pluripotent stem cells. These cells have the potential to form all the different cell types in the body and offer an exciting opportunity to develop new treatment strategies. Embryonic stem cells and induced pluripotent stem cells, however, are not good candidates to be used directly as treatments, as they require careful instruction to become the specific cells needed to regenerate diseased or damaged tissue. If not properly directed, these stem cells may overgrow and cause tumors when injected into the patient.
⚠ Caution: View clinics that offer the same cell treatment for a wide variety of conditions or diseases with extreme caution. Be wary of claims that stem cells will somehow just know where to go and what to do to treat a specific condition.
5. The science behind a disease should match the science behind the treatment.
The more you know about the causes and effects of your disease, the better armed you are to identify your best treatment options. If you have a certain type of blood cancer, for example, transplantation with blood-forming stem cells makes sense, as the treatment requires those specific cells to do exactly what they are designed to do. If you have diabetes, receiving a blood-forming stem cell treatment doesn’t make sense, because the problem is in the pancreas rather than in the blood itself. Without significant and careful manipulation in the lab, tissue-specific stem cells do not generate cell types found outside of their home tissues.
⚠ Caution: Your best protection against clinics selling unproven stem cell “treatments” is an understanding of the science behind your disease, injury or condition.
6. Cells from your own body are not automatically safe when used in treatments.
In theory, your immune system would not attack your own cells if they were used in a transplant. The use of a patient’s own cells is called an autologous transplant. However, the processes by which the cells were acquired, grown and then reintroduced into the body would carry risks. Here are just a few known risks of autologous stem cell treatments:
Any time cells are removed from your body, there is a risk they may be contaminated with viruses, bacteria or other pathogens that could cause disease when reintroduced.
Manipulation of cells by a clinic may interfere with their normal function, including those that control cell growth.
How and where the cells are put back into your body matters, and some clinics inject cells into places where they are not normally present and do not belong.
⚠ Caution: Every medical procedure carries risk; be wary of clinics that gloss over or minimize the risks associated with their treatments.
7. Patient testimonials and other marketing provided by clinics may be misleading.
It can be hard to tell the difference between doctors conducting responsible clinical trials and clinics selling unproven treatments. One common differentiator is the way a treatment is marketed. Most specialized doctors receive patient referrals, while clinics selling stem cell treatments tend to market directly to patients, often through persuasive language on the Internet, Facebook and in newspaper advertisements.
Clinics peddling unproven stem cell “treatments” frequently overstate the benefits of their offerings and use patient testimonials to support their claims. These testimonials can be intentionally or unintentionally misleading. For example, a person may feel better immediately after receiving a treatment, but the perceived or actual improvement may be due to other factors, such as an intense belief that the treatment will work, auxiliary treatments accompanying the main treatment, healthy lifestyle changes adapted in conjunction with the treatment and natural fluctuations in the disease or condition. These factors are complex and difficult to measure objectively outside the boundaries of carefully designed clinical trials. Learn more about why we need to perform clinical trials here.
⚠ Caution: Beware of clinics that use persuasive language, including patient testimonials, on the Internet, Facebook and newspapers, to market their treatments, instead of science-based evidence.
8. An experimental treatment offered for sale is not the same as a clinical trial.
The fact that a procedure is experimental does not automatically mean that it is part of a research study or clinical trial. Responsibly-conducted clinical trials are critical to the development of new treatments.
Responsible clinical trials share several important features:
They build upon their own preclinical data, lab-based research on cells, tissues and animals, that indicates the treatment being tested is likely to be safe and effective.
Oversight by an independent medical ethics committee to protect participant's rights.
Conformity to regulatory requirements, including a listing in a recognized clinical trial registry.
A structure designed to answer specific questions about a new treatment or a new way of using current treatments (results are usually compared with a control group of patients who do not receive the experimental treatment).
The cost of the new treatment and monitoring is not covered by the participant.
⚠ Caution: Beware of expensive treatments that have not passed successfully through clinical trials.
9. The process by which science becomes medicine is designed to minimize harm and maximize effectiveness
There is a lengthy, multi-step process involved in responsibly translating science into safe and effective medical treatments. During this process, scientists may discover that an approach that seemed promising in the lab, does not work in animals, or that an approach that worked in animals, does not work in humans. They may discover that a treatment effectively addresses symptoms of a disease or injury in humans, but that it carries unacceptable risks. Scientists carefully review and replicate their work, and invite their peers to do the same. This process by which science becomes medicine is often long, but it is designed to minimize patient harm and to maximize the likelihood of effectiveness.
⚠ Caution: Beware of clinics that circumvent the accepted process by which science becomes medicine.